
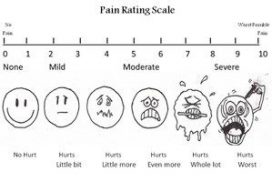
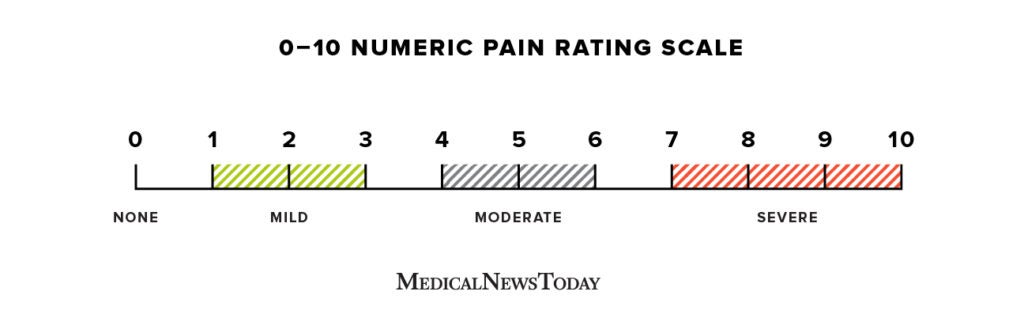
The importance of using the same numeric value (0-10) is that the number relates to the same pain intensity in each tool. All share a common numeric and recorded as values 0-10 and documented on the clinical observation chart as the 5th vital sign. Tools used for pain assessment at RCH have been selected on their validity, reliability and usability and are recognized by pain specialists to be clinically effective in assessing acute pain. Assess and document pain on activity such as physiotherapy.Assess and document pain before and after analgesia, and document effect.Children on complex analgesia such as intravenous opioid and/ or ketamine, epidurals or regional analgesia should have hourly pain and sedation scores documented.Children who are receiving oral analgesia should have pain scores documented at least 4 hourly during waking hours.Children with pain should have pain scores documented more frequently.Pain scores should be documented for all children at least once per shift in Flow Sheet: (.
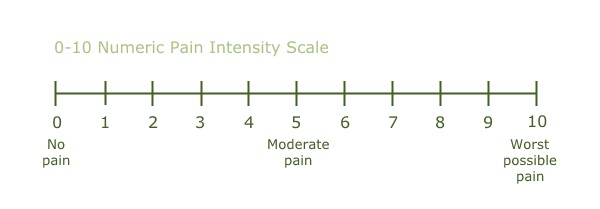
cognitive development and understanding of pain.Nursing Assessment nursing clinical guideline) Pain measurement quantifies pain intensity and enables the nurse to determine the efficacy of interventions aimed at reducing pain.Ī pain assessment should be conducted during a patient’s admission. Assessment and documenting pain is needed in order to improve management of pain. When assessing a child’s level of pain careful consideration needs to be given to their: In some children it can be difficult to distinguish between pain, anxiety and distress. The dependence on others to assess pain, limited language, comprehension and perception of pain expressed contextually. Pain assessment in infants and children is also challenging due to the subjectivity and multidimensional nature of pain. It is important to take behavioral cues identified by parents and caregivers to improve pain assessment in these children. However in children with developmental disabilities there can be incorrect assumptions and there is a risk of under-treating pain. Therefore physiological and behavioural tools are used in place of the self-report of pain. There are challenges in assessing paediatric pain, none more so than in the pre-verbal and developmentally disabled child. Pain assessment is a broad concept involving clinical judgment based on observation of the type, significance and context of the individual’s pain experience. Pain measurement tools: are instruments designed to measure pain. Pain assessment: is a multidimensional observational assessment of a patients’ experience of pain. “Pain is an unpleasant sensory and emotional experience, associated with, or resembling that associated with, actual or potential tissue damage” (IASP 2020).“Pain is whatever the experiencing person says it is, existing whenever the experiencing person says it does” (McCaffery, 1989).The guideline specifically seeks to provide nurses with information regarding In addition family response to their child in pain can have a negative or positive influence. Pain is multidimensional therefore assessment must include the intensity, location, duration and description, the impact on activity and the factors that may influence the child’s perception of pain (bio psychosocial phenomenon) The influences that may alter pain perception and coping strategies include social history/issues, cultural and religious beliefs, past pain experiences and the first pain experience. Acute pain (noiciception) is associated with tissue damage and an inflammatory response, it is self limiting of short duration and does not involve neural tissue. Pain is the most common symptom children experience in hospital. Nurses are in a unique position to assess pain as they have the most contact with the child and their family in hospital. Pain assessment is crucial if pain management is to be effective. For acute medical and surgical pain in children


 0 kommentar(er)
0 kommentar(er)
